
What’s Topical

Source: CMS
Last week, The Wall Street Journal reported that representatives from Elon Musk’s Department of Government Efficiency (DOGE) have gained access to the payment and contracting systems at the Centers for Medicare and Medicaid Services (CMS). Their primary objective is to evaluate CMS’s technology infrastructure and identify inefficiencies—with a key focus on reducing Medicare and Medicaid fraud, which the Department of Health and Human Services (HHS) estimated at over $86 billion in 2024.
DOGE’s investigation into Medicare and Medicaid payments could have significant implications for private equity, particularly in the outsourced revenue cycle management (RCM) industry—a sector that has seen substantial PE investment in recent years. Notable recent deals in the RCM space include:
- New Mountain’s acquisition of Access Healthcare for ~$2 billion (January 2025)
- TowerBrook and CD&R’s joint acquisition of R1 RCM for $8.9 billion (November 2024)
- EQT’s acquisition of GeBBS Healthcare Solutions for ~$850 million (September 2024)
What is Revenue Cycle Management?
Revenue Cycle Management (RCM) refers to the process by which healthcare providers (e.g., hospitals, clinics) capture, process, and optimize patient billing data to maximize collections—primarily from insurance companies, Medicare, and Medicaid—while minimizing delays in payment.
Because the process involves multiple complex and often manual steps, many healthcare providers outsource RCM operations to third-party specialists to improve efficiency and accuracy. The key steps in the RCM process are outlined below:

Source: Jorie AI
Patient Registration & Scheduling – Collecting accurate patient information and setting up appointments.
Insurance Verification & Authorization – Confirming insurance coverage and securing approvals for procedures.
Charge Capture – Assigning correct medical procedure and diagnosis codes to ensure accurate billing.
Billing & Claims Submission – Preparing and submitting clean claims to insurers, Medicare, and Medicaid while generating patient invoices.
Payment Processing – Managing reimbursements from payers and collecting patient payments.
Denial Management – Reviewing and addressing denied claims to prevent future issues.
Accounts Receivable Follow-up – Tracking and following up on unpaid charges to ensure timely collections.
Private Equity Investments in RCM
Private equity’s involvement in Revenue Cycle Management (RCM) dates back to the early 2000s, when Bain Capital, KKR, and Merrill Lynch Global Private Equity took HCA Healthcare private. While HCA primarily operated hospitals, PE ownership led to the creation of Parallon, a subsidiary that leveraged HCA’s internal RCM capabilities to provide outsourced RCM services to other healthcare providers.
The RCM industry has several attractive characteristics that continue to draw private equity investment:
🚀 Large market with significant outsourcing potential
The RCM market size varies across studies, but all estimates agree: it’s a huge and growing industry. According to Precedence Research, ~70% of RCM is still conducted in-house, leaving substantial room for growth for outsourced RCM providers.
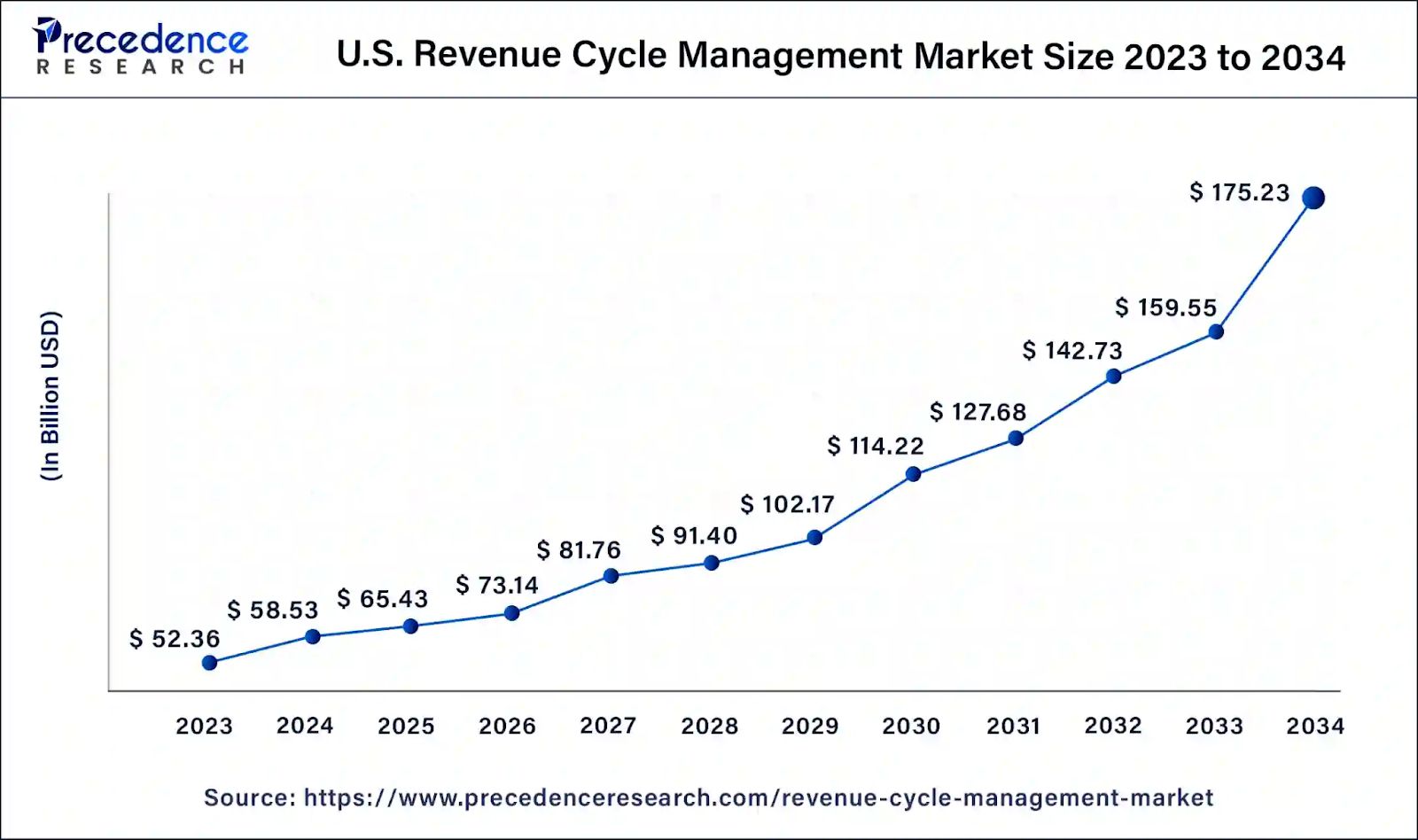
Source: Precedence Research
👩🏻⚕️ High employee turnover with opportunities to automate and offshore
RCM jobs are often manual, repetitive, and stressful, leading to industry-wide annual attrition rates of 20%+, with some companies experiencing 40-50% turnover. This high churn is driving:
Healthcare providers to outsource RCM to reduce staffing challenges.
RCM vendors to invest in AI, automation, and offshoring to streamline operations and bridge the talent gap.

Source: Healthcare IT Today
Looking Ahead: the DOGE Impact
While DOGE’s revamp of CMS’s technology and payment systems will take time—like all government initiatives—the eventual changes could have major consequences for outsourced RCM providers and the PE firms backing them.
🔧 Technology Overhauls Could Erase Competitive Advantages
Any CMS system upgrades will require RCM providers and healthcare facilities to undergo costly technology integrations and process overhauls. This could lead to major capital expenditures for RCM vendors and potentially eliminate any technological moat they’ve built.
💰 Reimbursement Structure Shifts May Disrupt Revenue Models
Changes in CMS processes and contractual terms could significantly alter Medicare/Medicaid reimbursements, impacting both healthcare providers and RCM vendors. Since RCM firms typically charge a percentage of cash collected from insurers/Medicare/Medicaid, any shift in reimbursement dynamics could have direct revenue implications.
While RCM has been a lucrative sector for PE firms—evidenced by ChrysCapital’s ~5x exit of GeBBS Healthcare to EQT in 2024—the uncertainty surrounding DOGE’s involvement creates new risks for future investors.
That’s a wrap on this week’s Weekly Roll-Up. See you Saturday with another Deep Dive!
RATE TODAY’S EDITION
If you enjoyed the newsletter, please share with friends and subscribe at https://perollup.beehiiv.com/subscribe